Against the Current, No. 111, July/August 2004
-
Empire of Lies and Torture
— The Editors -
Race and Class: Brown v. Board of Education 50 Years Later
— Malik Miah -
A Future Sacrificed for War
— Nomi Prins -
The Fight to Save Kevin Cooper
— Todd Chretien -
Trophy Photographs
— Kevin Cooper -
South Africa's Deadly Decade of HIV Denial
— Patrick Bond -
Chinese Workers' Resistance
— Norm Diamond interviews Tim Pringle -
Korean Labor: Protest by Suicide
— Sang-Hwan Jang -
British Labour Today
— Liam Mac Uaid -
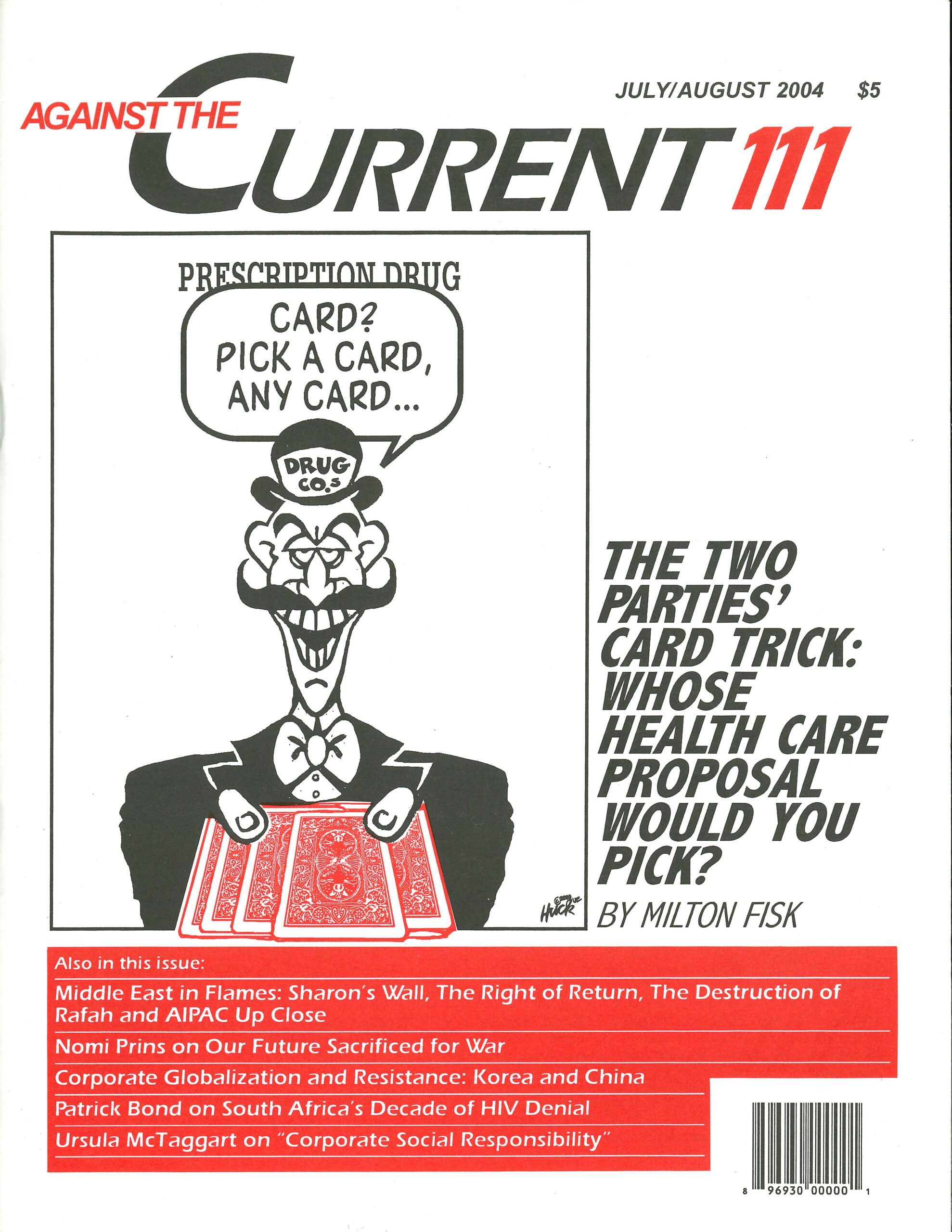
The Health Care Crisis and Kerry-Bush
— Milton Fisk -
The Mythology of Corporate Social Responsibility
— Ursula McTaggart -
Random Shots: Save That Scrap Metal
— R.F. Kampfer - Middle East in Flames
-
Bush-Sharon's Hell on Earth
— David Finkel -
A Slice of Death in Rafah
— from an International Solidarity Movement report -
The Nightmare Comes True
— Uri Avnery -
The Right of Return & Transformative Justice
— Yoav Peled -
The Lobby Up Close & Personal
— Henry Herskovitz - More Dialogue on the Elections
-
Winning 2004 & Beyond
— Brian Sandberg -
A Case for Nader Now
— Jeff Melton -
Rejoinder: 2004 & the Movement
— Christopher Phelps, Stephanie Luce & Johanna Brenner - Reviews
-
The End of Guzzlemainia
— Michael Livingston -
The Poetry of J. Quinn Brisben
— Angel Martinez - In Memoriam
-
Remembering Paul Siegel (1916-2004)
— Alan Wald
Patrick Bond
THE AFRICAN NATIONAL CONGRESS has returned to power with an overwhelming majority in South Africa’s third post apartheid democratic election. With millions of South Africans dying early because of AIDS, however, the question posed in the header of this article remains, along with a broader one:
In the wake of ten years of HIV/AIDS denialism, can deadly structural forces—namely, capitalist incentives to allow millions of disposable non workers to die, unnecessarily—also be overcome?
The battle against the disease was one of the most crucial tests of the ANC government. Its systematic failure to address AIDS, and especially its ongoing sabotage of medicinal treatment for HIV+ patients, led to periodic charges of ‘genocide’ by authoritative figures such as the heads of the Medical Research Council (Malegapuru William Makgoba), SA Medical Association (Kgosi Letlape), and Pan Africanist Congress health desk (Costa Gazi), as well as leading public intellectual Sipho Seepe.
Aside from president Thabo Mbeki, Pretoria’s main saboteurs were health minister Manto Tshabalala Msimang and trade minister Alec Erwin; the latter two were accused by the Treatment Action Campaign (TAC) of culpable homicide during a March 2003 civil disobedience campaign.
Even in the weeks before the 2004 election, Mbeki and Tshabalala Msimang continued to practice denialism, obfuscation, delays, bureaucratic maneuvers and withdrawal of resources for treatment. Educational campaigns were based upon fatuous marketing to hip hop youth, and virtually nothing was done to combat domestic violence, rape, multiple partners and patriarchy.
Across Africa more generally, the ‘ABCs’ of abstinence, being loyal and condoms were particularly ineffectual within the confines of male dominated marriage, leading to the tragedy that the young women’s infection rate was twice as high as that of men.
A great deal has been written about Pretoria’s malfeasance. The point of revisiting it here is to provide a structural explanation for the crisis. Beyond the oft cited peculiarities of the president himself, there are three deeper reasons why local and global power relationships meant that the battle against AIDS has mainly been lost, to date.
One reason is the pressure exerted by international and domestic financial markets to keep Pretoria’s state budget deficit to 3% of GDP. Recall the telling remark of the late Parks Mankahlana, Mbeki’s main spokesperson, who in March 2000 justified to Science magazine why the government refused to provide relatively inexpensive anti retrovirals (ARVs) like Nevirapine to pregnant, HIV positive women:
That mother is going to die and that HIV negative child will be an orphan. That child must be brought up. Who is going to bring the child up? It’s the state, the state. That’s resources, you see. (Quoted in Mail and Guardian, 21 July 2000)
Instead of saving lives, Mbeki’s finance ministry adopted higher priorities: slashing corporate taxes; redeploying state resources to purchase high tech arms; and repaying roughly $25 billion worth of apartheid era foreign debt and a bit more in apartheid domestic debt, which could have been declared ‘Odious’ in legal terms. Such examples of fiscal laxity the local and international bankers generally approved, in contrast to expanding state health spending and other social budgets, which the bankers have explicitly not supported.
The second structural reason is the residual power of pharmaceutical manufacturers to defend their rights to ‘intellectual property,’ i.e. monopoly patents on life saving medicines. This pressure did not end in April 2001 when the Pharmaceutical Manufacturers Association withdrew their notorious lawsuit against the South African Medicines Act of 1997.
That Act allows for parallel import or local production, via ‘compulsory licenses,’ of generic substitutes for brand name anti retroviral medicines. Big Pharma’s power was felt in the debate over essential drugs for public health emergencies at the November 2001 Doha World Trade Organization summit, and ever since.
The third structural reason for the ongoing HIV/AIDS holocaust in South Africa is the vast size of the reserve army of labour, for this feature of capitalism allows companies to replace sick workers with desperate, unemployed people instead of providing them treatment.
Corporate Incentives to Deny Treatment
The latter point deserves elaboration, simply because so many lives are at immediate risk, and because so much evidence has mounted that corporate South Africa’s preferred approach has been, in essence, mass murder by denial of medical benefits. This was the initial conclusion reached after a year of internal study at Africa’s largest company, Anglo American Corporation.
Anglo has 160,000 employees, of whom 21% are estimated to be HIV+. Once Big Pharma appeared to retreat from its lawsuit, the company announced it would provide anti retroviral medicines (ARVs) to its workforce, which meant literally tens of thousands of lives might be saved in the short term.
But in June 2001, the Financial Times reported on Anglo’s plans to make special payments to miners suffering from HIV/AIDS, on condition they take voluntary retirement. However, in addition to bribing workers to go home and die, Anglo told the FT, “treatment of employees with anti retrovirals can be cheaper than the costs incurred by leaving them untreated.”
In August, Anglo’s vice president for medicine, Brian Brink, bragged in Business Day about a “strategy [which] involved offering wellness programmes, including access to anti retroviral treatment.” According to that report, “The company believed that the cost of its programmes would eventually be outweighed by the benefits its received in gradual gains in productivity, [Brink] concluded. Although it was indeed a risky strategy, it was the only one Anglo could pursue in the face of such human suffering.”
Then in October 2001, Anglo simply retracted its promise, once cost benefit analysis showed that 146,000 workers just weren’t worth saving. According to the FT, Brink “said the company’s 14,000 senior staff would receive anti retroviral treatment as part of their medical insurance, but that the provision of drug treatment for lower income employees was too expensive.”
Brink explained the criteria for the fatal analysis: “[Anti retrovirals] could save on absenteeism and improved productivity. The saving you achieve can be substantial, but we really don’t know how it will stack up. We feel that the cost will be greater than the saving.”
As the Wall Street Journal (April 16, 2002) recorded, “In a controversial move that could have wide ramifications for how companies in poor countries handle AIDS, mining giant Anglo American PLC has put on hold a feasibility study to provide AIDS drugs to its African work force, according to people familiar with the situation. When it disclosed its plans for the study a year ago, Anglo garnered wide praise because it was one of the first major corporations to reveal measures aimed at treating AIDS cases among its rank and file African employees.”
Anglo changed its mind once again a few months later, as AIDS ravaged the middle layer of the workforce, and the multi class TAC raised consciousness sufficiently high as to get trade union support for member treatment.
But the need for hard nosed capitalist cost benefit analysis was expressed again by financier George Soros, when he was asked about treating HIV positive South Africans in an April 2002 interview with the SA Broadcasting Corporation. He answered, “I think to provide treatment to the bulk of the people is just not feasible. I think to provide treatment for instance to qualified workers actually saves money, actually saves money for companies.”
Interviewer Ben Cashdan responded, “Aren’t you uncomfortable to talk in a way that is a kind of death sentence to those who we can’t afford to treat?” Replied Soros, “I think the cost of providing actual treatment to everyone at the present—I don’t think it’s realistic. It’s not achievable.”
Fear of Demonstrators
In the cases of both Anglo and Coca Cola, the other factor that appeared in 2002 was the specter of consumer protest over the firms’ refusal to treat employees. For Anglo, I was reliably informed by insiders, the prospect of demonstrators at the August 2002 World Summit on Sustainable Development dragging up many other bits of dirty laundry intimidated the company executives into taking preemptive action on the AIDS front.
Coke’s main bottler in South Africa had also failed to insure two thirds of its 4,000 strong workforce at a sufficient level to allow the HIV+ workers access to ARVs, and was subject to international protest over African AIDS policies.
However, even though the costs of HIV/AIDS—absenteeism, declining productivity, payouts for early death—soared to as high as 25% of payroll by 2003, according to the Financial Times, most employers are still hesitant to provide ARVs:
FT, 18 September 2003)
In sum, no matter the effectiveness of activism against government, Big Pharma and the corporate employers, all three structural factors are still deterrents to provision of treatment. By late 2003, each was slightly mitigated, however, and that led to an ostensible change of policy by Pretoria.
The budget deficit was projected to climb from just over 1% of GDP during the early 2000s to nearly 3% in 2004 05, allowing extra leeway for AIDS spending. Pharmacorps were cooperating more closely with the World Health Organization, the Global Fund, the Clinton Foundation and governments to lower prices for Africa.
Canada’s former prime minister Jean Chretien—spurred by the dynamic, outspoken UN advisor Stephen Lewis—even introduced pathbreaking legislation to promote generic drugs (although a sabotage clause was later included in the draft law to support patent rights, in turn attracting a new round of solidarity protests). And employers began waking up, in part because of the dramatic rise of AIDS related disability claims as a percentage of all disability claims, from 18% in 2001 to 31% in 2002.
These factors converged in a November 2003 Cabinet statement, finally endorsing a roll out of anti retrovirals. Pretoria cited factors which included:
A fall in the prices of drugs over the past two years. New medicines and international and local experience in managing the utilisation of ARVs. [sufficient] health workers and scientists with skills and understanding. And the availability of fiscal resources to expand social expenditure in general, as a consequence of the prudent macro economic policies pursued by government.
These factors were minor, however, compared to intensive activist pressure, which Pretoria did not dare mention lest it encourage further protests.
After the Activist Victory
TAC’s victory statement was explicit:
The combination of the Constitutional Court decision on mother to child transmission prevention, the Stand Up for Our Lives march [of 15,000 people on parliament] in February, the civil disobedience campaign and the international protests around the world have convinced Cabinet to develop and implement an ARV rollout plan.
Another factor, of course, was the 2004 presidential election, which Mbeki would win easily but which would be characterized by high levels of apathy and no vote campaigning by the Landless Peoples Movement.
An AC Nielsen survey in November 2003 confirmed that Mbeki’s AIDS policy was hurting the ruling African National Congress’ chances of turning out the vote. The Cabinet statement promised that “within a year, there will be at least one service point in every health district across the country and, within five years, one service point in every local municipality.”
In addition to medicines, the state would provide an education and community mobilization program, promotion of good nutrition and traditional health treatments such as herbal remedies, support for families affected by HIV and AIDS, and funds for upgrading health infrastructure.
The health system was already massively overextended, with far too few essential medicines, much less ARVs, available in South Africa’s underfunded rural clinics.
As TAC was the first to concede, ARV availability could generate negative unintended consequences. One would be noncompliance with treatment regimes by poor people, and the concomitant emergence of drug resistant strains. Another would be the black market smuggling of cheap drugs to Europe and North America, which would reduce access in Africa.
Another is that although stigmatization will decline given the availability of hope giving drugs, so too might the practice of safe sex. These would remain major challenges to TAC and other health sector groups, although Medicins sans Frontiers’ Khayelitsha operation was already proving high levels of treatment compliance.
Moreover, the conflict between neoliberalism and life, so explicit in the case of access to AIDS medicines, was severely compounded by patriarchy, traditional and modern sexual practices such as multiple partners for men, and domestic violence against women. Rape continued at scandalous levels.
But the primary contradiction involved the regime in Pretoria. In February 2004, the TAC attacked President Thabo Mbeki in the wake of more government prevarication on AIDS treatment. Claiming that Mbeki “misrepresented facts and once again caused confusion on HIV/AIDS” on national television, TAC’s Zackie Achmat accused him of “denialism.”
The Government’s Conduct
Moreover, Pretoria had originally promised to distribute AIDS medicines to at least 50,000 people within a year, and to reach everyone in need of treatment within five years. Health Minister Tshabalala Msimang blamed slow drug procurement—Pretoria’s own fault—and the lack of qualified health personnel.
Commented TAC strategist Mark Heywood, “Many hospitals have the capacity, they just don’t have the medicines.” The finance ministry also cut the budget required for medicines purchases dramatically in February 2004.
At the same time, Tshabalala Msimang suggested that while HIV positive people waited for medicines, a diet of lemons, beetroot, (extremely expensive) olive oil and garlic would improve the body’s immune system.
A week earlier, the minister had come under fire by the SA Medical Association, whose chairperson Dr Kgosi Letlape accused her of “dividing the profession when we have gone to great lengths to unite it.” The minister unsuccessfully attempted to halt a protest march of 2000 medics, against poor conditions in public health facilities, by implying that the demonstrating doctors were white, whereas black medics supported the government.
Mbeki continued supporting his minister, no matter how outrageous this became. He told the SA Broadcasting Corporation on February 8, 2004, that the major problem was inaccurate mortality statistics which made it impossible to know whether AIDS was as fatal as claimed.
According to Mbeki, his doctors informed him that diabetes is also an epidemic, and he questioned why no one talked about diabetes. Replied Achmat:
Drugs for treating diabetes are heavily overpriced; there should be a campaign for their reduction. But unlike HIV until November 2003, diabetes is treated in the public health sector. However, the President should be aware that according to an initial investigation into the burden of disease estimates in South Africa released in 2003 by the Medical Research Council, AIDS was responsible for 39% of lost life years in 2000—more than the next 10 worst diseases. Diabetes is the 12th worst disease and is responsible for slightly more than 1% of lost life years. The two diseases are incomparable in scale.
In addition, Achmat ridiculed Mbeki’s claim that “few countries can hold a candle to South Africa’s HIV/AIDS program.” In reality, Achmat replied:
A number of developing countries do much better than South Africa when it comes to HIV prevention and treatment, often with far fewer resources. Currently, South Africa treats approximately 1,500 people in its public sector, who are not on drug trials, paying for their own medicines or being sponsored. By contrast, Brazil’s government treats over 100,000 people and has less than a quarter of South Africa’s HIV infections. Botswana is treating approximately 15,000 and Cameroon approximately 7,000 people.
In March 2004, the need to harass Pretoria to ensure roll out was confirmed again, when TAC had to prepare an urgent court interdict so as to permit the urgent acquisition of antiretroviral medicines consistent with the November 2003 Cabinet decision.
Tshabalala Msimang was sufficiently threatened by yet more embarrassing legal proceedings that she finally agreed, just before a deadline provided by TAC lawyers. TAC declared victory, though remarking that “by implementing the interim procurement mechanism and thereby avoiding a three month delay of the treatment program, approximately 6,000 excess deaths could [have been] avoided.”
Continuing Struggle and Hope
What way forward, given the persistent presidential denialism, state bureaucratic sabotage, and structural factors that mitigated against treatment access? One major stumbling block would probably emerge in subsequent months and years: the nature of political alliances within South Africa.
TAC had been effective in attracting support from the most forward looking trade unions, the SA Communist Party, churches, NGO activists and technical supporters (lawyers, health workers, academics, journalists). Yet these alliances did not stray far from the ANC.
Would TAC forge sufficient linkages to non ANC communities (especially those devoted to building the new independent left)? In coming years, would the myriad of problems that cause AIDS opportunistic infections—especially dirty water and air (thanks to coal/wood/paraffin)—also be addressed?
At a time when the South African government was disconnecting water and electricity at a lethal rate, alongside evictions for those who could not afford expensive rental and mortgage bond payments, the need to address links between AIDS and diseases of poverty/homelessness was obvious.
Moreover, would TAC and its allies make the case that access to ARVs is a human right and that people should not pay user fees or partial cost recovery for the medicines? By 2004, they were taking this position, but only in the event that people were too poor to pay for medicines. Yet ‘means testing’ of black South Africans with irregular informal incomes is notoriously difficult.
In contrast, a more explicit ‘free lifeline’ strategy would parallel the demands of the water and electricity campaigners.
Nevertheless, whether or not TAC continues to tackle the three structural impediments to ARV access—neoliberal fiscal policy, pharmacorps and corporate control of health perks—the immediate victory of access to medicines will potentially make a huge difference.
For the half million South Africans who are symptomatic with AIDS or who have a CD4 blood count less than 200, there was suddenly hope. Across the world, for three million people who die each year of AIDS, and for 40 million others infected, the treatment activists and their international allies deserve a standing ovation.
ATC 111, July-August 2004