Against the Current, No. 206, May/June 2020
-
A Crisis of Vast Unknowns
— The Editors -
Virus Is Color Blind, Not Humans
— Malik Miah -
UC Graduate Student Workers Wildcat Strike
— Shannon Ikebe -
Two-Tier Response to COVID-19
— Ivan Drury -
Producing Knowledge for Justice
— Rabab Abdulhadi -
On the Delhi Pogrom
— Radical Socialist, India -
Class Struggle and the Pandemic
— Kunal Chattopadhyay -
Introduction to William Z. Foster and the TUEL
— The ATC Editors -
TUEL and the Rank-and-File Strategy
— Avery Wear -
A New Economy Envisioned?
— Dianne Feeley - Reviews
-
A Bitter Class Grudge War
— Rosemary Feurer -
The GI Bill, Then and Now
— Steve Early -
Vagabonds of the Cold War
— John Woodford -
A Problematic Diagnosis
— Michael Tee -
Hidden Deaths in a Long War
— Barry Sheppard -
Hugo Blanco's Revolutionary Life
— Joanne Rappaport -
Karl Marx in His Times
— Michael Principe -
Karl Marx in His Times
— Michael Principe - In Memoriam
-
Gene Francis Warren Jr., 1941-2019
— Ron Warren -
Socialism as a Craft
— Mike Davis
Malik Miah
THE CORONAVIRUS IS color blind. It strikes whites, Blacks, Latinos, indigenous people, Asians, rich and poor. So why the higher number of cases and deaths for African Americans?
Structural inequality and racism explain why African Americans are dying at a much higher rate than whites in the COVID-19 pandemic.
Permanent color-based inequality is developed out of a system of white supremacy that predates the Revolutionary War in 1776. The colonies under English rule considered Africans, whether enslaved or “free,” as inferior to whites. After Independence, the ideology of white supremacy remained and persists to the present.
That original crime is why the worldwide COVID-19 pandemic kills African Americans more than twice the rate as for whites. The invisible enemy does not discriminate, only humans do.
Many white Americans are surprised by a colorblind disease. They had always assumed that Blacks dying from other viruses and diseases was their own fault. “It’s them, not us.” Today, the fear is that high death rates for African Americans could be a signal to greater deaths for them.
African Americans with underlying health conditions face permanent inequalities in their daily lives (a structural racial deficit), suffer more and die at greater numbers than whites.
The Data
Statistics (from a selection of states) show this life gap. As of this writing (April 12):
Illinois: Blacks are 15% of the state’s population, whites 77%. Deaths: 42% Black, 36% white.
Michigan: Blacks are 14% of state’s population and 40% of deaths (heavily concentrated in the metro area of Detroit. The three counties of metro Detroit make up 83% of the state’s deaths).
Mississippi: Blacks are 38% of state’s population, 72% of deaths.
Louisiana: Blacks are 33% of the population, 70.5% of deaths.
South Carolina: Blacks are 27% of the population, 46% of the deaths.
New York City (the epicenter of the virus): Blacks and Hispanics die at twice the rate of whites, who are 46% of the population. The racially diverse Elmhurst section of Queens is being devastated.
Official figures are underestimated, as New York City has not counted deaths of many people who died at home and were never taken to hospitals. There were not enough tests to check.
Some of this racial disparity is tied to specific type of jobs that Black men and women can get such as transit, garbage collection, postal delivery, home care and nurses’ aides in public health. Internet access and computers are less plentiful in low-income homes. Diabetes, hypertension and asthma are prevalent.
The Centers for Disease Control and Prevention (CDC) charts the racial gap in all walks of life for Blacks and whites before the Covid-19 virus:
Life expectancy: 74 years for Blacks; 79 years for whites.
Infant mortality rate before age one per 1000 births: 11.5 for Blacks; 6.17 for whites. Both infant and maternal mortality are even higher in African American majority cities like Detroit.
Obesity in the United States: At all ages it is almost twice as high for African Americans. Specifically from ages 20-39 years, Blacks 46%, whites 26%. Obesity is a form of malnutrition, and access to quality affordable food is a big factor.
Hypertension is a major risk factor for heart disease, heart attack and stroke: Some 75% of Blacks develop high blood pressure, compared to just 55% of white men and 40% of white women.
Housing segregation: Despite fair housing laws Blacks continue to be excluded from housing loans (or at much higher mortgage rates) and programs through redlining and discrimination.
Freed Blacks after the Civil War (1861-65) were denied land and property; before and after WWII many new housing programs prioritized suburban development and did not grant favorable loans to Blacks, even though many served in the military.
Unemployment (Bureau of Labor Statistics): It is twice as high for African Americans than white Americans — some 6.3% in 2018 for Blacks, 3.3% for whites — obviously before the current economic collapse. (This does not count those who stopped looking for jobs, those working part time or those so-called independent contractors such as Uber drivers.)
The Detroit Story
Benjamin Wallace-Wells observes in his article “Inequality intensifies coronavirus crisis in Detroit”:
“We are just beginning to see demographic data on those who’ve died of covid-19, but African-American communities around the country may be especially vulnerable…
“In Detroit, where seventy-nine per cent of the population is Black and thirty-six per cent is below the poverty line, the diabetes rate is roughly twice the national average. Southeastern Michigan has become a national epicenter of the outbreak, and though African Americans are just fourteen per cent of the state’s population they represent forty-one per cent of itscovid-19 victims…
[Dr Rana] Awdish and her colleagues [at Henry Ford Hospital, in midtown Detroit, one of the largest teaching hospitals in the country] are on the front lines in two senses: in Detroit, the pandemic is escalating in intensity, and poverty and poor health may be changing its shape.” (New Yorker, April 7)
The United States is the only developed country in the world where there is no universal health care. The racial gap, however, has prevented united action — even though most people now support a single payer type system. Blacks, Latinos and Native Americans have never received fair and equal treatment. Many African Americans don’t have a primary care physician.
The ideology of white supremacy is so engrained that solidarity between whites and others has been difficult to forge. Racial inequality is exacerbated under a system that puts business and profits first. Yet the need for health solidarity is changing that.
Inequality Spreads COVID-19
The same is true for inequality around the world. Racial conflicts have undermined development and anti-capitalist struggles, including in Africa and Latin America.
“Why inequality could spread COVID-19,” by Faheem Ahmed, Na’eem Ahmed, Christopher Pissarides and Joseph Stiglitz in the British medical publication The Lancet (April 2) explains:
“Estimates indicate that COVID-19 could cost the world more than $10 trillion, although considerable uncertainty exists with regard to the reach of the virus and the efficacy of the policy response.
“For each percentage point reduction in the global economy, more than 10 million people are plunged into poverty worldwide. Considering that the poorest populations are more likely to have chronic conditions, this puts them at higher risk of COVID-19-associated mortality.
“Since the pandemic has perpetuated an economic crisis, unemployment rates will rise substantially and weakened welfare safety nets further threaten health and social insecurity.”
In short, people in less developed regions such as Africa with weak health systems and safety nets will be hit the hardest.
Opportunity for United Action
An opportunity nevertheless exists today. To close the inequality gap is possible as more working-class people and farmers see the virus as color blind. Many whites who had ignored racism now express some solidarity to minorities dying at higher numbers.
As 22 million Americans lose their jobs in the first month and then lose their employer-based health insurance, the demand for a Medicare-for-all health care system seems logical. U.S. law does not pay for sick leave or provide other basic social services as other wealthy countries do.
More whites and most African Americans are asking, “Why not?” As the Federal Reserve prints trillions of dollars to save the economy, what were once seen as “socialist” demands seems more and more realistic.
How to win is also clearer: mass action by working people for fundamental changes to the system that put profits before health. The invisible enemy is showing that unity is possible, and that the essential driver of the economy is not capital but labor.
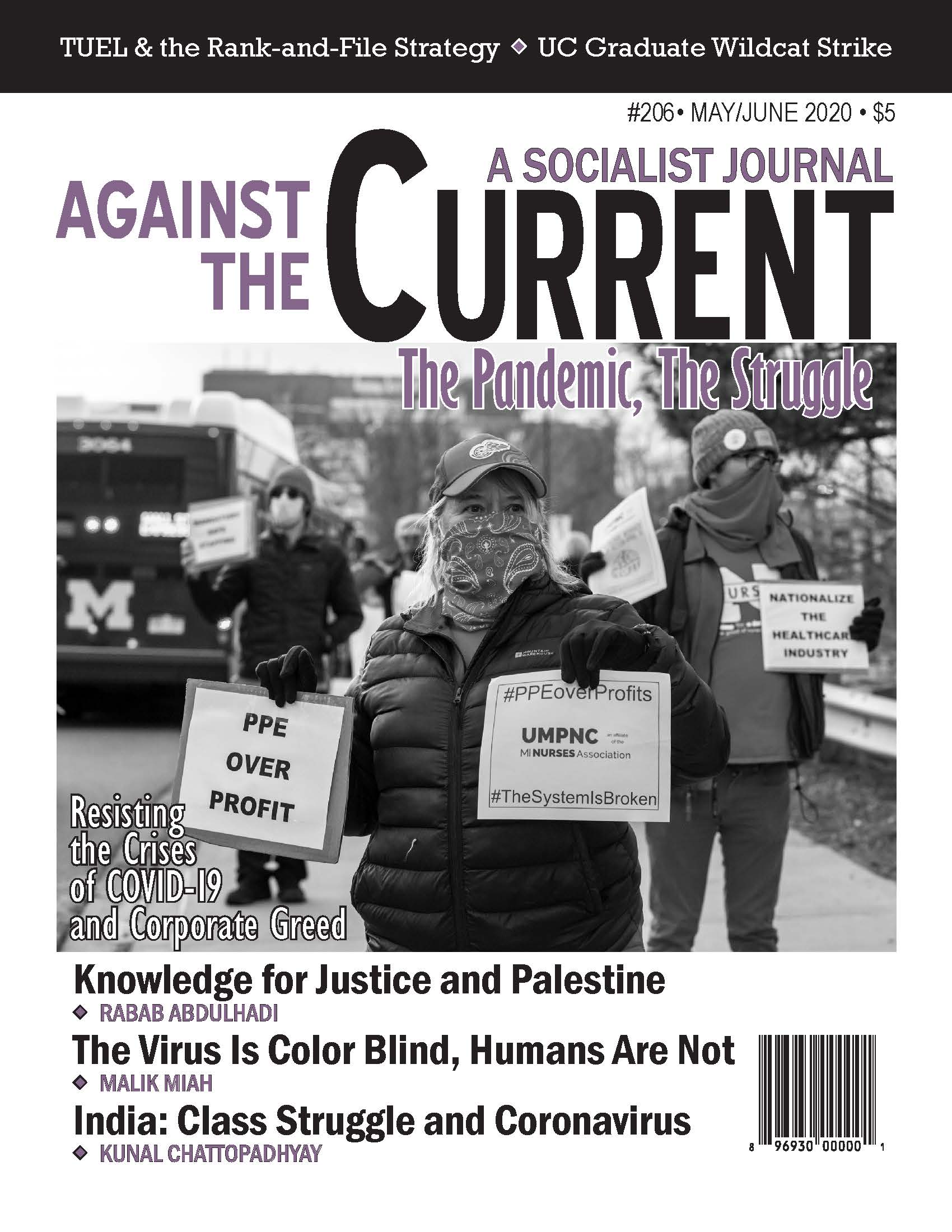
The demand for nationalization of the health care and drug industries for the public good is more realistic than ever. A new radical leadership is possible, and necessary.
May-June 2020, ATC 206